Can You Be Allergic To Seminal Fluid: Everything You Need To Know In 2026
Picture this: Sarah and Mark, a couple head-over-heels, enjoying a particularly intimate moment. Everything is going swimmingly, if you catch my drift, until suddenly… ouch. Not the fun kind of ouch, but a stinging, burning, downright uncomfortable kind of ouch. Sarah, utterly bewildered, starts to feel itchy and then… well, let's just say the mood definitely took a nosedive. It wasn't an STI, tests came back clean. So, what on earth was happening? Was she suddenly allergic to… Mark?
It sounds a bit wild, right? Like something out of a bizarre medical drama. But turns out, this isn't some fictional plot twist. This is the reality for a surprising number of people who can, in fact, be allergic to seminal fluid. And no, it’s not just a “he’s just a bit sensitive” situation. This is a genuine, albeit rare, medical condition, and by 2026, we’re hopefully a lot more clued up about it. So, let’s dive deep, shall we? No pun intended… okay, maybe a little.
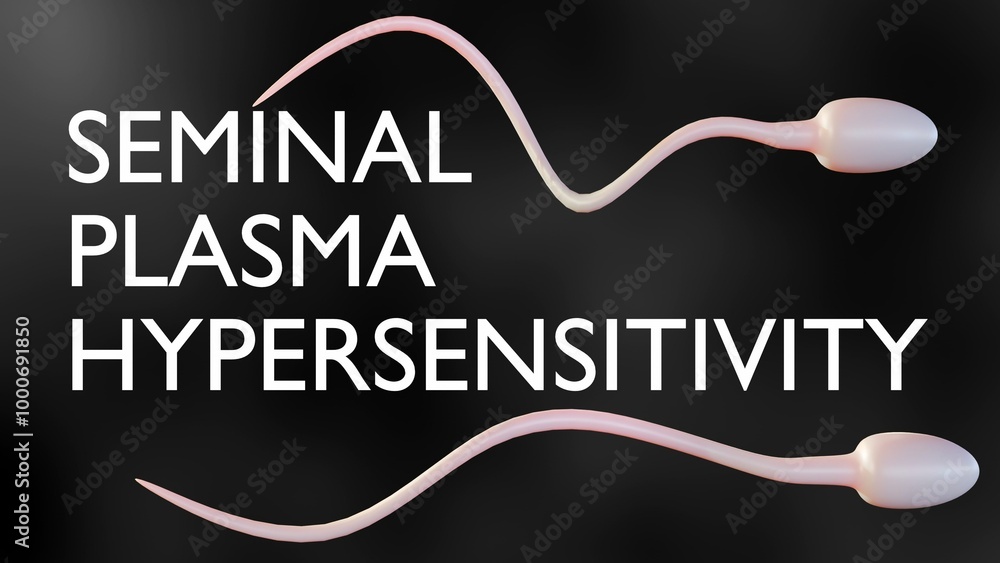
The Uncomfortable Truth: Seminal Plasma Hypersensitivity
So, the official, fancy medical term for this is seminal plasma hypersensitivity (SPH). Catchy, right? It basically means your body’s immune system is having a bit of a freak-out over something present in the semen. And it’s not just the sperm itself, which is a common misconception. It’s often the proteins in the seminal plasma – the liquid part of semen – that trigger the allergic reaction.
Think of it like a mild case of pollen allergy, but instead of sneezing when a bee buzzes by, you’re reacting to… well, you know. And it can happen to anyone, regardless of gender. While it’s often discussed in the context of cisgender women reacting to their male partners’ semen, cisgender men can also experience SPH, and it's something that can affect individuals of any sexual orientation or gender identity. It’s a surprisingly diverse phenomenon, if you think about it.
Who’s More Likely to Get It? (And Why Are We Only Hearing About It Now?)
Honestly, identifying specific risk factors is still a work in progress, even in 2026. It’s not like you can get a genetic test for it (yet!). However, some research suggests that individuals with a history of other allergies might be more susceptible. If you’re already sneezing your way through spring and breaking out in hives from that new laundry detergent, your immune system might just be a tad… overenthusiastic.
The reason we’re hearing more about it now, and will continue to in 2026, is multi-faceted. Firstly, there's a growing awareness and destigmatization around sexual health. People are more willing to talk about these kinds of issues, which is fantastic! Secondly, medical research is getting more sophisticated. We're better equipped to diagnose and understand these less common conditions.
Historically, it was probably brushed off as something else – irritation, a mild infection, or even psychosomatic. But as our understanding of immunology and reproductive health expands, SPH is finally getting the attention it deserves. It's about time we acknowledge that our bodies can react in unexpected ways, especially when it comes to something as complex as sexual intimacy.
Symptoms: The Not-So-Fun Signals Your Body Sends
So, what does this allergic reaction actually look like? It can vary wildly from person to person, and even from encounter to encounter. Some people have very mild reactions, while others experience pretty significant discomfort. It’s not exactly a subtle hint from your body, let’s be real.
Common symptoms can include:

- Localised itching or burning: This is probably the most frequent and immediate reaction. You might feel it right after contact, or within a few minutes.
- Redness and swelling: The affected area can become red, inflamed, and even a bit swollen. Think of it like a mild sunburn, but in a… more sensitive area.
- Rash or hives: Some individuals develop a rash or hives on the skin that has come into contact with the semen.
- Pain or discomfort: Beyond the itching, there can be a general feeling of soreness or pain.
- Vaginal dryness or irritation: For those with vaginas, this can lead to dryness, burning, and general discomfort, making intercourse painful.
- Less commonly, systemic reactions: In very rare cases, more severe, systemic allergic reactions can occur, such as difficulty breathing or a drop in blood pressure. This is serious and requires immediate medical attention.
It’s important to note that these symptoms can sometimes mimic other conditions, like yeast infections or bacterial vaginosis. This is why getting a proper diagnosis from a healthcare professional is absolutely crucial. Don’t self-diagnose, okay? Your body is a complex machine, and sometimes it needs a professional mechanic.
When Does It Typically Show Up?
SPH can manifest at any point in a person's life. You could be perfectly fine for years, then suddenly develop an allergy. Or it could appear shortly after becoming sexually active. There's no strict timeline, which can make it all the more confusing and frustrating to deal with. It’s like your body decided to change the rules of the game mid-play. Totally fair.
Sometimes, the symptoms might be so mild that they are overlooked or attributed to other causes, like friction or a bit of rough play. But as the years go by, and if the person continues to be exposed, the sensitivity can sometimes increase. This is where it might become more noticeable and disruptive.
Diagnosis: The Detective Work of Your Doctor
Figuring out if you have SPH is a bit like being a detective. Your doctor will be looking for clues, gathering evidence, and ruling out other suspects. It's not as simple as a quick swab for an STI. You’ll likely need a combination of methods.
The Medical History and Physical Exam
This is the starting point. Your doctor will ask you a lot of questions about your sexual history, your symptoms, when they started, and how they manifest. They'll also perform a physical exam to check for any visible signs of irritation or inflammation. Be prepared to be very open and honest – they’re there to help, not judge!
Ruling Out Other Culprits
This is a biggie. As mentioned, SPH symptoms can overlap with other issues. So, your doctor will likely conduct tests to rule out:

- Sexually Transmitted Infections (STIs): This is a top priority. A standard STI screening is usually the first step.
- Yeast Infections: These are common and can cause similar itching and irritation.
- Bacterial Vaginosis (BV): Another common cause of vaginal discomfort.
- Contact Dermatitis: You could be reacting to something else, like lubricants, condoms, or even laundry detergent.
- Prostatitis: In men, inflammation of the prostate can cause discomfort.
It’s a process of elimination, and it can take time. So, try to be patient with the process, even if it’s frustrating. You want to make sure you’re getting the right diagnosis for the right problem.
Allergy Testing: The Gold Standard (But Not Always Easy)
The most definitive way to diagnose SPH is through allergy testing. This usually involves:
- Skin Prick Testing: In this method, a small amount of diluted seminal fluid (obtained from a willing donor, often the partner, or sometimes synthesized in a lab) is pricked into the skin. A positive reaction (a raised, itchy bump) indicates a potential allergy.
- Intradermal Testing: Similar to skin prick testing, but the allergen is injected just under the skin. This is often more sensitive.
- Patch Testing: Less common for SPH, but sometimes used if a contact allergy is suspected.
Now, here’s where it gets a bit tricky, especially in the past (though hopefully less so by 2026). Obtaining a safe and standardized sample of seminal fluid for testing can be a challenge. Not all clinics have the resources or protocols for this. Furthermore, some individuals might react to the diluent used in the testing, leading to a false positive. It requires a skilled allergist who is experienced in this specific area. Don’t be surprised if you have to do a bit of searching to find a doctor who can perform these tests effectively.
Treatment and Management: Living with SPH
The good news is that even if you are diagnosed with SPH, it doesn’t necessarily mean the end of a satisfying sex life. Management strategies exist, and by 2026, we're likely to have even more refined options.
Avoidance (The Obvious, But Not Always Practical)
The most straightforward way to avoid a reaction is to avoid contact with seminal fluid. Obviously, this has implications for conceiving naturally and for sexual intimacy. For some, this might mean choosing not to have penetrative sex or relying on barrier methods.
Barrier Methods: The First Line of Defense
Condoms are the go-to for many. They create a physical barrier between the seminal fluid and the sensitive tissues. However, it’s not always a foolproof solution.
Some individuals might still react to the latex or lubricants in condoms, or even to minute amounts of seminal fluid that might leak. In these cases, non-latex condoms (like polyurethane or polyisoprene) and hypoallergenic lubricants might be a better option. It’s all about finding what works for you and your partner.
Desensitization Therapy: The Long Game
This is where things get really interesting and have seen significant advancements by 2026. Vaginal desensitization therapy, also known as hyposensitization, is a form of allergy treatment. It involves introducing tiny, gradually increasing amounts of seminal fluid to the vaginal tissues over time.
The goal is to retrain the immune system to tolerate the proteins in the seminal plasma. This is usually done under the strict supervision of a healthcare professional, often in a clinical setting. It can be a lengthy process, requiring commitment and patience from both partners, but it can be highly effective for many.
Imagine this: starting with a minuscule amount of fluid, perhaps diluted to the point where it’s almost undetectable, and slowly, over weeks or months, increasing the concentration. It’s like teaching your body to be less dramatic about its reactions. This therapy is a testament to how far we've come in understanding and treating allergies.
Antihistamines and Topical Treatments
For milder reactions, over-the-counter antihistamines can help manage itching and redness. Your doctor might also prescribe topical creams or ointments to soothe irritated skin. These are often used to manage symptoms and provide relief, rather than curing the underlying allergy.
Alternative Conception Methods
For couples who wish to conceive naturally, SPH can present a significant challenge. However, there are still options.
- Intrauterine Insemination (IUI): In this procedure, the seminal fluid is washed to remove the seminal plasma proteins, and only the sperm are used for insemination. This can be a viable option for many.
- In Vitro Fertilization (IVF): IVF involves fertilizing the egg outside the body. Again, the seminal fluid is processed to isolate the sperm.
These assisted reproductive technologies are lifesavers for many couples facing fertility issues, including those complicated by allergies. It’s amazing how science can bridge these gaps.
The Partner's Role: It's Not Just About You!
If you’re the one experiencing SPH, it’s easy to feel isolated or even embarrassed. But remember, your partner is likely going through this with you. Their understanding, support, and willingness to explore management strategies are absolutely vital.
Open communication is key. Talk about how you’re feeling, both physically and emotionally. Your partner can be your biggest ally in navigating this. They might also be the one to initiate conversations about seeking medical help or trying new approaches.
It’s a team effort. And honestly, navigating challenges like this together can often strengthen a relationship. It forces you to be vulnerable, to communicate, and to find solutions as a unit. Plus, who knows? You might discover a whole new level of intimacy and trust.
Looking Ahead: What to Expect in 2026 and Beyond
As we look towards 2026, the landscape of understanding and managing SPH is continually evolving. We can anticipate:
- Increased Awareness and Education: More people will be aware of SPH, leading to earlier diagnosis and less unnecessary distress.
- Improved Diagnostic Tools: We might see more standardized and accessible allergy testing methods.
- Refined Treatment Options: Research into desensitization therapies and potentially even pharmacological interventions will likely lead to more effective treatments.
- Greater Support Networks: Online communities and support groups will likely flourish, providing a space for individuals to share experiences and advice.
It's a journey, and one that requires ongoing research and open dialogue. The more we talk about it, the more we normalize it, and the better we can support those who are affected.
So, to recap: yes, you can be allergic to seminal fluid. It’s a real condition with real symptoms. But it’s also a manageable one. With the right diagnosis, support, and treatment plan, a fulfilling and intimate life is absolutely within reach. And by 2026, we’re hoping to be even better equipped to handle it. Now, go forth and be informed, and remember, your body is amazing, even when it throws you a curveball!
