Can You Take Out Of Date Antibiotics: The Truth, Facts, And What To Expect

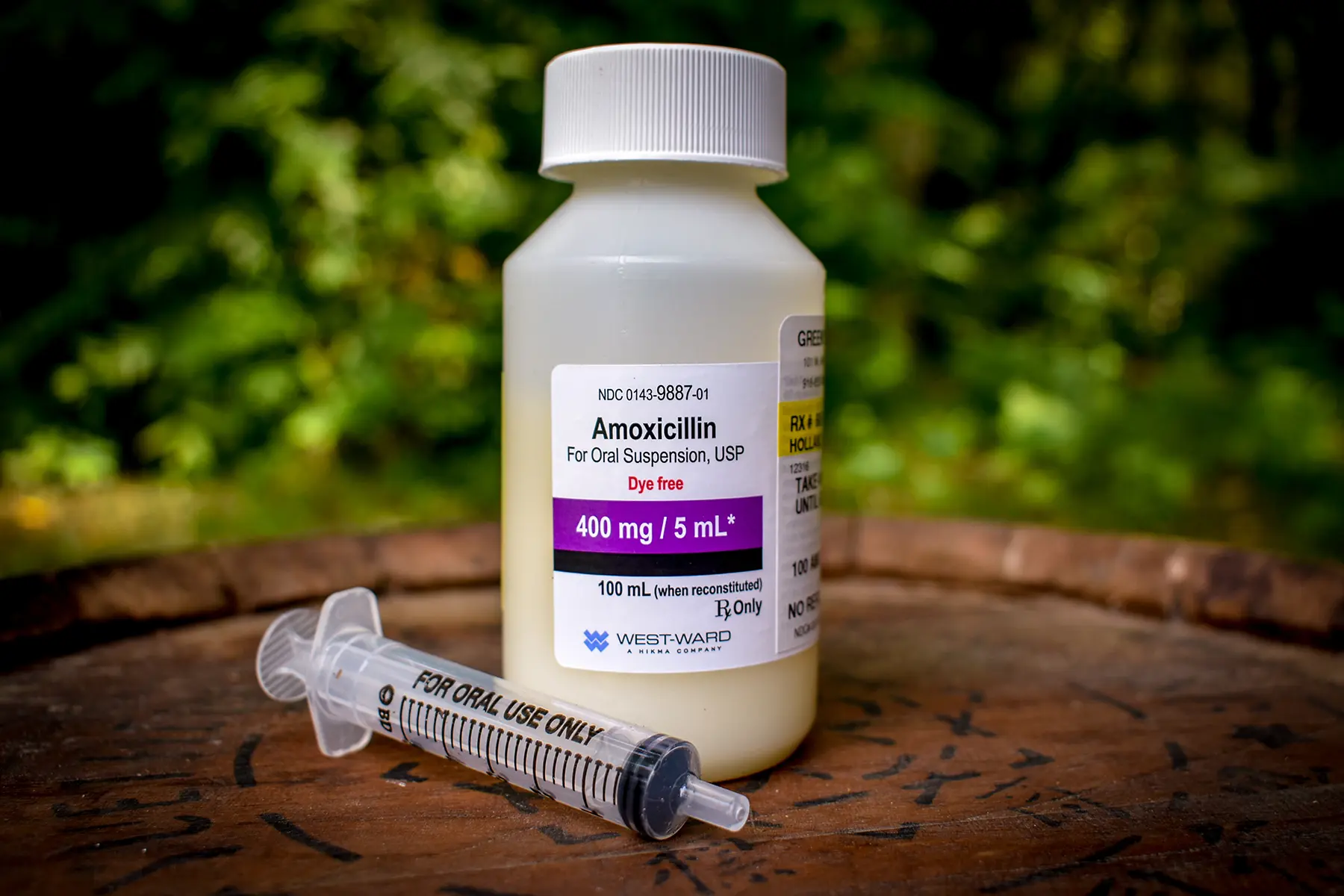
Picture this: It’s 3 AM. You’re shivering, your throat feels like sandpaper, and your head is pounding a rhythm only a true plague victim could appreciate. Your trusty bathroom cabinet, usually a beacon of hope for minor ailments, is your last resort. You rummage through it, past the expired ibuprofen and the weirdly sticky band-aids, and then you spot it. A small bottle of antibiotics, a leftover from that nasty ear infection you had… a couple of years ago. The expiry date? Well, it’s definitely in the rearview mirror. Suddenly, a thought pops into your feverish brain: “Can I still take these?”
Oh, the age-old question, right? We’ve all been there, staring at that little bottle, weighing the desperate need for relief against the shadowy fear of… well, what exactly? Is it going to turn into poison? Will it magically work anyway? Or is it just… going to do nothing at all? It’s like a medical gamble, and honestly, who wants to gamble with their health when they’re feeling this lousy? Let’s dive into the nitty-gritty of out-of-date antibiotics, the truth, the facts, and what you might actually expect.
The Expiration Date: Why Do They Even Bother?
So, first things first, why do we have these pesky expiration dates on our medications anyway? It’s not like milk that suddenly turns into a science experiment in your fridge. Pharmaceutical companies are legally required to put an expiration date on their drugs. This date is essentially a promise, a guarantee from the manufacturer that the medication will remain potent and safe up until that point, assuming it’s stored correctly, of course. Think of it as a “best by” date for your medicine. After that date, they can’t officially vouch for its quality.
This isn’t just some arbitrary number they pull out of a hat. It’s based on rigorous testing that determines how the drug degrades over time under various conditions. Factors like temperature, humidity, and light can all play a role in breaking down the active ingredients. So, while your antibiotic might not suddenly become toxic, its effectiveness could definitely take a nosedive.
The Big Question: Do Out-Of-Date Antibiotics Still Work?
This is where things get interesting, and also, a little bit fuzzy. The simple answer is… it depends. Generally speaking, most medications, including antibiotics, tend to lose their potency over time. The active ingredients can degrade, meaning you might not get the full therapeutic dose you need to fight off that nasty bacterial infection. And when it comes to antibiotics, this is a huge deal.
Imagine you’re battling a bacterial invasion. You need an army of antibiotic warriors to take down the enemy. If your antibiotic warriors are old and tired, they might not be strong enough to win the fight. You might end up with a lingering infection, or worse, the bacteria could develop a resistance to that particular antibiotic. This is a major public health concern, and something doctors and scientists are constantly battling. So, taking a weakened antibiotic could inadvertently contribute to the growing problem of antibiotic resistance. Nobody wants that, right?
The Science Behind the Slow Fade
The chemical compounds in antibiotics are designed to be stable, but they're not invincible. Over time, they can undergo chemical changes. This can mean a reduction in the concentration of the active drug. So, if your prescription was for 500mg of an antibiotic, an expired pill might actually contain less than that. And as we mentioned, when you’re trying to kick a bacterial infection, every milligram counts.
It’s not like they suddenly become useless overnight. The degradation is usually gradual. So, a few months past the expiry date might not make a huge difference, whereas several years might render them practically inert. But again, it’s a gamble, and the stakes are pretty high. You’re not just playing with your own well-being; you’re potentially impacting the effectiveness of antibiotics for future infections, for yourself and for others.
What Happens If You Take Them Anyway? The Potential Pitfalls
Okay, so we’ve established they might not be as potent. But what else could go wrong? This is where the fear-mongering in our heads sometimes kicks into overdrive. Let’s break down the actual risks, rather than the dramatic movie scenarios.
1. Ineffectiveness (The Most Likely Scenario): This is the most common outcome. The antibiotic simply won’t be strong enough to kill the bacteria. This means your symptoms might not improve, or they could even get worse. You’ll still feel sick, and the infection will continue to fester. Not ideal when you’re already feeling miserable.
2. Antibiotic Resistance: This is the big one. When you take a sub-therapeutic dose of an antibiotic (meaning, not enough to kill all the bacteria), the surviving bacteria can learn to fight it off. They become resistant. This means that the next time you get a similar infection, that same antibiotic might not work anymore. And this resistance can spread to other people and other types of bacteria. It’s a vicious cycle, and it’s one of the biggest threats to global health. Seriously, it’s not a joke.
3. Side Effects (Less Common, But Possible): While the primary concern is reduced effectiveness, there's also a small chance that the degraded components of the antibiotic could cause unexpected side effects. This is less likely with most common antibiotics, but it’s not entirely impossible. Think of it like food – sometimes something slightly past its date can cause digestive upset, even if it doesn’t look or smell off. The same principle can apply, albeit in a much more complex way, to medications.

4. Unpredictability: The biggest issue is simply that you don’t know what you’re getting. The expiry date is a marker of quality control. Without it, you’re flying blind. You can’t be sure of the dosage, the potency, or even if the chemical structure has changed in a way that could be harmful.
The Medical Consensus: Just Don't Do It
So, what do the experts say? Unsurprisingly, the overwhelming consensus from doctors, pharmacists, and health organizations is a resounding “No.” They strongly advise against taking expired antibiotics.
Why the firm stance? It all comes back to efficacy and the looming threat of antibiotic resistance. They would rather you go to the doctor, get a proper diagnosis, and be prescribed a fresh, potent course of antibiotics than risk a failed treatment and the development of resistance. It’s about protecting your health and the broader public health.
Think about it from their perspective. They are trained to use specific medications at specific doses to achieve specific outcomes. Taking an unknown quantity of a potentially weakened drug throws a massive wrench into that well-oiled machine. It’s like a mechanic trying to fix your car with rusty, mismatched tools. It’s not going to end well.
When the "Rules" Seem Flexible: The Exception to the Rule?
Now, I know what you might be thinking. “But I’ve heard stories! My uncle’s friend’s cousin swore by their expired antibiotics!” And yes, anecdotes abound. There are even some anecdotal accounts of medications, particularly those with a very long shelf life like tetracycline, showing minimal degradation over a few years. Some sources even suggest that in dire, life-or-death situations where no other options are available, a slightly expired medication might be a last resort.

However, and this is a huge however, these are extreme exceptions, and often not based on solid scientific evidence for the specific antibiotic in question. Relying on these stories is a dangerous game. The vast majority of antibiotics, especially liquid forms or those that are sensitive to heat and light, will degrade significantly. Furthermore, what might be a mild infection for one person could be a severe, life-threatening one for another. You just don’t know.
The reality is that the risks associated with taking expired antibiotics (ineffectiveness, resistance, potential side effects) far outweigh any perceived benefit, especially when a perfectly valid and safe alternative exists: consulting a healthcare professional.
So, What's the Best Course of Action?
When faced with that expired bottle of antibiotics, the best course of action is to safely dispose of them and seek professional medical advice. Seriously, this is the golden rule.
Safe Disposal: Don't just flush them down the toilet or throw them in the trash where they can contaminate the environment or be found by someone else. Most pharmacies have medication take-back programs. You can also check with your local waste management facility for guidelines on how to dispose of medications safely. It’s a small step that makes a big difference.
See a Doctor or Pharmacist: If you’re feeling unwell, especially with symptoms that suggest a bacterial infection (fever, severe pain, pus, etc.), your first port of call should be your doctor or a walk-in clinic. They can properly diagnose your illness and prescribe the appropriate medication. If you’re unsure about a medication you have, whether it’s expired or not, a pharmacist is an invaluable resource. They can offer guidance on proper storage, dosage, and when a medication is no longer safe or effective.
Think of it as an investment in your health. A doctor’s visit might seem like an inconvenience when you’re feeling rough, but it’s a sure way to get you on the road to recovery with the right tools. And honestly, the peace of mind knowing you’re taking a safe and effective medication is priceless.
Storage Matters: Keeping Your Meds Fresh
While we’re on the topic, let’s talk about how to prevent this situation in the first place. Proper storage is key to maximizing the shelf life of your medications. Most antibiotics should be stored in a cool, dry place, away from direct sunlight and moisture. Avoid keeping them in the bathroom medicine cabinet, as the humidity from showers can degrade them over time. The kitchen cupboard or a drawer in your bedroom is often a better bet.
And always, always check the expiry dates when you’re putting away new medications. It’s a good habit to get into. If you know you have a history of certain infections, ask your doctor if it's appropriate to keep a course of antibiotics on hand with clear instructions and a short expiry date to monitor. But this is a conversation to have with your healthcare provider, not a DIY approach.
The Bottom Line: When in Doubt, Throw It Out (and See a Doctor)
So, to circle back to our 3 AM feverish dilemma, can you take out-of-date antibiotics? The honest, evidence-based answer is you shouldn't. The potential for reduced effectiveness, the significant risk of contributing to antibiotic resistance, and the general unpredictability of taking degraded medication make it a gamble that’s simply not worth taking.
Your health is too important, and the fight against antibiotic resistance is too critical, to mess around with expired drugs. It’s tempting, I get it. That feeling of wanting to be your own doctor and solve a problem quickly is powerful. But in this case, the DIY approach can have serious repercussions. So, next time you find yourself staring at that aged antibiotic bottle, resist the urge. Dispose of it properly, and then take a deep breath, and make that appointment. Your body, and future generations of bacteria-fighting medicine, will thank you for it.
