Taking Antibiotics And Probiotics At Same Time: Complete Guide & Key Details
So, there I was, feeling like a walking petri dish. A nasty bug had decided my gut was its new vacation destination, and let's just say it wasn't a pleasant stay. My doctor, bless her understanding soul, prescribed a course of antibiotics. "Take these diligently," she said, her voice firm but kind. I nodded, already envisioning the sweet relief. But then, a little voice in my head, probably fueled by late-night internet scrolling, piped up: "Wait a minute... what about the good guys?" You know, the friendly bacteria that normally keep everything in my belly humming along like a well-oiled machine. Were these antibiotics going to evict them too? This whole antibiotics-and-probiotics-at-the-same-time conundrum is something I bet more than a few of you have pondered while staring into the abyss of your medicine cabinet. And honestly, it's a legit question! Let's dive into it, shall we?
Because, let's be real, the idea of taking two seemingly opposing forces at once can feel a bit like trying to pat your head and rub your belly simultaneously. One's a warrior, ready to obliterate invaders, and the other's a peacekeeper, trying to maintain a delicate ecosystem. So, can they coexist? Do they cancel each other out? Or, dare I hope, can they actually help each other?
This is where we get to unpack the whole "antibiotics and probiotics together" dance. It’s a topic that sparks a lot of curiosity, and for good reason! We’ve all been told antibiotics are lifesavers, but we’ve also heard whispers (and seen more than a few glossy ads) about probiotics being our gut's best friends. So, what’s the deal when they share the stage?
The Antibiotic Gauntlet: Why We Need Them (and the Side Effects)
First off, let's give credit where credit is due. Antibiotics are pretty darn amazing. They're like the superheroes of the medical world, swooping in to fight off dangerous bacterial infections that our bodies, left to their own devices, might struggle with. Think strep throat, nasty UTIs, or even more serious stuff. Without them, many common illnesses would be far more life-threatening. So, a huge, grateful thank you to science for these powerful drugs!
But, and this is a big "but," these bacterial warriors are not exactly picky eaters. While they're busy annihilating the bad guys, they often don't discriminate. They can also take a serious toll on the good bacteria that live in our gut, on our skin, and elsewhere. It's like sending in the army and having them accidentally flatten the local village along with the enemy stronghold. Not ideal, right?
This collateral damage is what leads to some of the most common (and annoying!) side effects of antibiotics. Ever had that chalky, upset stomach after a course of antibiotics? Or experienced some… digestive disruptions that make you want to hide in the bathroom for days? Yep, that's often the good bacteria crying out in protest. They're essential for digestion, nutrient absorption, and even immune function. When they're wiped out, things can get… messy.
It’s like a perfectly balanced orchestra where suddenly the violins decide to take an impromptu vacation, leaving the percussion section to do all the work. Things get loud, unbalanced, and frankly, a little chaotic. And that, my friends, is where our probiotic pals come in, or at least, where the idea of them comes in.
Enter the Probiotics: The Gut's Friendly Villagers
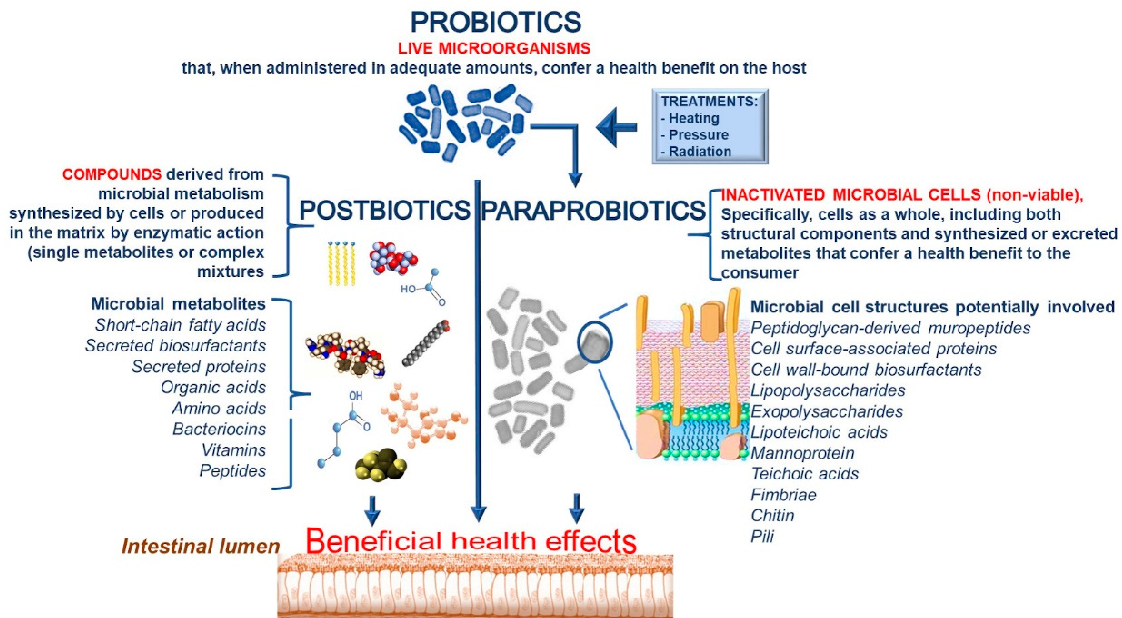
Now, let's chat about probiotics. Think of them as the hardworking, helpful citizens of your internal city. These are live microorganisms, primarily bacteria (but sometimes yeasts!), that, when consumed in adequate amounts, confer a health benefit on the host. Basically, they're the good guys, the ones we want hanging around and doing their thing. They help break down food, produce vitamins, and crucially, they help keep the more mischievous or outright harmful microbes in check. They're the peacekeepers, the community organizers, the ones who throw a good party to keep morale high.
You find these friendly bacteria naturally in fermented foods like yogurt with live and active cultures, kefir, sauerkraut, kimchi, and kombucha. And of course, they're readily available as dietary supplements. Their reputation has grown immensely, and for good reason. They play a vital role in maintaining a healthy gut microbiome, which is increasingly linked to everything from mood to immunity.

So, if antibiotics are like the demolition crew, and probiotics are the rebuilding crew, why wouldn't we have them work together? It seems like a no-brainer, right? Let's get to the nitty-gritty of whether this strategy actually works.
Can You Take Antibiotics and Probiotics at the Same Time? The Big Question
The short answer? Yes, you generally can, and in many cases, it's actually recommended! But, as with most things health-related, there are nuances, and it’s always best to get personalized advice from your doctor. Don't just blindly grab both from the shelf without a thought, okay? Think of this as a guide to having an informed chat with your healthcare provider.
The idea behind taking probiotics alongside antibiotics is pretty straightforward: to help mitigate the damage that antibiotics can inflict on your gut flora. While the antibiotics are busy doing their job, the probiotics are there to try and replenish the good bacteria or at least keep them from being completely decimated. It's like having reinforcements on standby.
Imagine your gut as a garden. Antibiotics are the weed killer, very effective at getting rid of the unwanted plants. But they might also damage some of the beneficial flowers. Probiotics are like the seeds you sprinkle in, hoping they'll take root and grow, filling in the gaps left by the weed killer and helping the garden flourish again quickly.
When to Take Them: Timing is Everything (Sort of)
This is where things get a little more specific, and you'll often hear different advice. The general consensus, and what most studies suggest, is to stagger your doses. Why? Because if you take them too close together, there's a theoretical risk that the antibiotic could kill the very probiotics you're trying to introduce.
So, what's the magic formula? Most experts recommend taking your probiotic at least 2 to 3 hours apart from your antibiotic dose. For example, if you take your antibiotic at 8 AM, you might take your probiotic around lunchtime (say, 1 PM or 2 PM) and then your next antibiotic dose in the evening (around 8 PM). This gives the antibiotic time to do its work on the bacteria it's targeting without immediately clashing with the probiotic supplement.
Think of it like this: you wouldn't want your welcome party for new guests to be immediately interrupted by a riot, right? You want the guests (probiotics) to settle in before the (theoretical) disruption happens. So, giving them that buffer zone is key.
Some people even suggest taking probiotics on days you don't take antibiotics, but if you're on a short course, that might not be enough to get the benefits. The most common and practical advice is the staggered dosing. It's a small adjustment that can make a big difference.
Which Probiotics Are Best When You're on Antibiotics?
Not all probiotics are created equal, and when you're dealing with the big guns of antibiotics, you want to choose wisely. The research points to specific strains that have shown particular promise in preventing or reducing antibiotic-associated diarrhea (AAD). The most commonly cited and well-researched strains include:
- Lactobacillus rhamnosus GG (LGG): This is a star player! It's one of the most studied probiotics and has shown great efficacy in preventing AAD in both children and adults.
- Saccharomyces boulardii: This is actually a beneficial yeast, not a bacterium, but it functions similarly in the gut. It's been shown to be very effective in preventing antibiotic-associated diarrhea and other gastrointestinal issues.
- Certain other Lactobacillus and Bifidobacterium strains: While LGG and S. boulardii are often highlighted, a good multi-strain probiotic that includes a variety of these beneficial bacteria can also be helpful. Look for products that list specific strains rather than just "probiotic blend."
When you're choosing a probiotic, look for reputable brands that clearly label the strains and colony-forming units (CFUs). The higher the CFUs, generally the more potent the probiotic, but the specific strain matters more than just a sky-high number. Again, your doctor or pharmacist can be a great resource here!
The Benefits: Why Bother?
Okay, so we've established you can take them together, and there's a specific way to do it. But what's the payoff? Why go through the extra effort?
The primary benefit is preventing or reducing antibiotic-associated diarrhea (AAD). This is the big one. AAD can range from mild inconvenience to severe, debilitating diarrhea that can sometimes lead to more serious complications. Probiotics, especially the ones mentioned above, can significantly lower your risk of experiencing this unpleasant side effect. It's like having a protective shield for your gut.
Beyond diarrhea, a healthy gut microbiome is linked to:

- Improved nutrient absorption: When your good bacteria are balanced, they help you get the most out of your food.
- Stronger immune function: A significant portion of your immune system resides in your gut. A healthy gut means a more robust immune response.
- Better mood and mental health: The gut-brain connection is a hot topic, and a balanced microbiome is thought to play a role in mental well-being.
- Reduced risk of other infections: A robust gut flora can act as a barrier against pathogens.
So, it’s not just about avoiding a nasty tummy ache; it's about supporting your overall health during and after antibiotic treatment. It’s about ensuring that while you’re fighting off one unwelcome guest (bacteria), you’re not leaving your internal home vulnerable to a whole host of other problems.
Potential Downsides and Who Should Be Cautious
While generally safe, taking probiotics, especially during antibiotic treatment, isn't entirely without potential considerations. For most healthy individuals, the risks are minimal, but it's good to be aware.
Mild digestive upset: Some people might experience gas, bloating, or mild stomach discomfort when they first start taking probiotics. This usually subsides as your body adjusts. It’s like your gut inhabitants are having a bit of a housewarming party, and things can get a little rowdy at first!
Interactions with specific antibiotics: While the general advice is to stagger doses, in rare cases, there might be specific interactions. This is why consulting your doctor is so important. They know your medical history and the specific antibiotic you're prescribed.
For immunocompromised individuals: This is a crucial point. If you have a severely weakened immune system (due to conditions like HIV/AIDS, undergoing chemotherapy, or post-organ transplant), you must discuss probiotic use with your doctor. In very rare instances, beneficial bacteria could potentially cause an infection in severely immunocompromised individuals. Your doctor will weigh the risks and benefits very carefully.
For those with serious illnesses: If you have a serious underlying medical condition, again, your doctor's guidance is paramount. They can advise on the most appropriate course of action for your specific situation.
Essentially, the advice is to be an informed patient and partner with your healthcare provider. Don't be afraid to ask questions! It’s your health, and you deserve to understand what’s going on.
When to Stop Probiotics After Antibiotics
The general recommendation is to continue taking probiotics for at least a week or two after you finish your course of antibiotics. This helps give your gut microbiome a chance to fully recover and re-establish a healthy balance. Think of it as a follow-up maintenance crew.
Some people choose to continue taking probiotics long-term, especially if they find they experience ongoing digestive benefits or if they have conditions that are known to benefit from probiotic support. Others might just use them proactively whenever they have to take antibiotics. It’s really about what works best for your body and your individual health needs.
The goal is to help your gut bounce back stronger. You've put it through the wringer with the antibiotics, and giving it a little extra support afterwards is a smart move. It’s like giving your garden a good watering and some fertilizer after a harsh storm.
The Bottom Line: A Partnership for Gut Health
So, there you have it. The seemingly complicated dance of antibiotics and probiotics can actually be a harmonious partnership. When used correctly, with proper timing and thoughtful selection, probiotics can be a valuable ally in mitigating the side effects of antibiotic treatment and supporting your overall gut health.
Remember, this isn't medical advice, and you should always consult with your doctor or pharmacist before starting any new supplement regimen, especially when you're already on prescription medication. They can help you choose the right product and ensure it's safe for you. But hopefully, this guide has demystified the topic a bit and empowered you to have a more informed conversation with your healthcare provider. Your gut will thank you!
And hey, if you’ve ever tried this combo yourself, I’d love to hear about your experience in the comments below! Did it help? What did you take? Let’s share our wisdom, because, after all, we’re all in this gut-health journey together, one friendly bacterium at a time!
