What Happens If You Take Birth Control When Pregnant: Complete Guide & Key Details

So, you’re wondering, what’s the deal with taking birth control if you’re already pregnant? It’s a question that pops into people’s minds, and honestly, it’s a pretty interesting scenario to explore. Think of it like accidentally putting salt in your coffee instead of sugar – you might be a little surprised by the result, and there’s a whole story behind it!
Let’s dive in, shall we? No need for panic buttons or dramatic music. We’re just here to get curious and understand what’s going on.
The Big Question: Can You Take Birth Control When Pregnant?
Okay, so the short and sweet answer is: it’s generally not recommended and, frankly, usually unnecessary. Birth control’s whole job is to prevent pregnancy, right? So, if you’re already pregnant, its primary function is sort of… done for the current situation. It’s like trying to lock the barn door after the horse has already bolted. It doesn't really serve its intended purpose anymore.
But what if someone did take it, either by mistake or before they even knew they were pregnant? That’s where things get a bit more nuanced and, dare I say, scientifically fascinating!
Mistakes Happen, Knowledge Grows
Imagine this: you’re on a regular birth control schedule, and you just haven’t taken a pregnancy test yet. You pop your pill, unaware of the tiny miracle developing inside. Or maybe you’re switching methods and there’s a small overlap. Life is messy, and these things can occur.
So, what happens to the developing baby when mom is taking birth control? This is the core of our curiosity.

The Science Bit (Made Easy!)
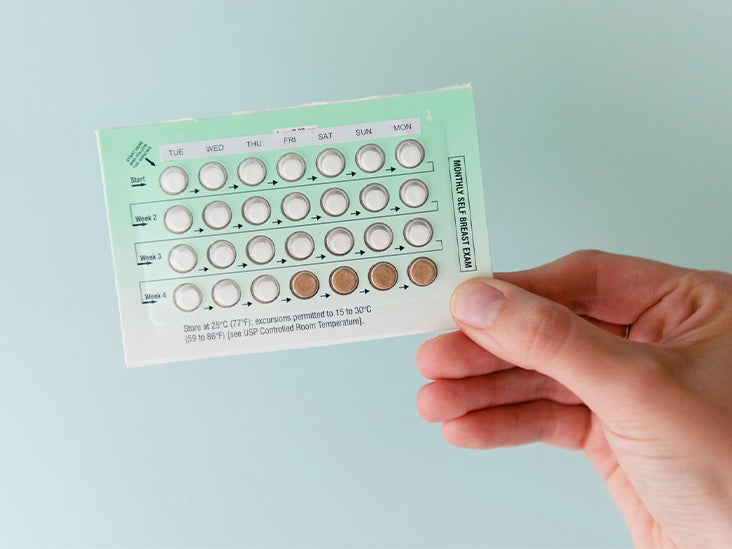
Birth control pills, patches, rings, and injections primarily work in a few ways:
- Stopping ovulation: They prevent your ovaries from releasing an egg.
- Thickening cervical mucus: This makes it harder for sperm to reach the egg.
- Thinning the uterine lining: This makes it harder for a fertilized egg to implant.
Now, if you're already pregnant, ovulation has already happened, and likely, fertilization and implantation have too. So, the preventative mechanisms of the birth control are no longer actively needed or effective in stopping the pregnancy itself.
So, Is It Harmful?
This is the biggie, right? The question on everyone’s mind. The good news, and this is a significant piece of good news, is that most studies have shown that taking hormonal birth control before you know you're pregnant does not significantly increase the risk of birth defects.
Think of it like this: the hormones in birth control are similar to the hormones your body is already producing during pregnancy. While the amounts might be different, they're generally in the same ballgame. It’s not like you’re suddenly introducing a completely foreign and potentially toxic substance into your body.
Doctors and researchers have looked into this quite a bit, and the consensus is reassuring. The hormones in most birth control methods (like estrogen and progestin) are not considered teratogenic, meaning they are unlikely to cause major birth defects. It's like pouring a little extra water into a river that’s already flowing strong – the river can handle it.
What About Different Types of Birth Control?
We’re mostly talking about hormonal methods here. But what about non-hormonal options? If someone were to, for example, have an IUD (intrauterine device) in place when they became pregnant, that’s a different scenario. An IUD’s primary function is to prevent pregnancy from even starting. If pregnancy occurs with an IUD in place, it’s considered an ‘intrauterine pregnancy’, and the IUD might need to be removed by a healthcare professional to reduce risks like infection or miscarriage. This is definitely something to discuss with your doctor immediately.
But back to the hormonal pills and such. The key takeaway is that if you find out you’re pregnant and you’ve been taking your birth control, the most important thing is to stop taking the birth control and contact your healthcare provider.

Why Stop?
Even if it’s not causing harm, there are good reasons to stop:
- It’s no longer serving its purpose. Why continue taking medication you don't need?
- Potential for side effects. Like any medication, birth control can have side effects. If you don't need it, why risk those?
- Medical monitoring. Your doctor will want to monitor your pregnancy closely, and stopping the birth control is part of that initial guidance.
The “Oops, I’m Pregnant and Still on Birth Control” Scenario
So, you took that pregnancy test, and it’s positive. You also remember you’ve been diligently taking your birth control pills. Deep breaths! It’s okay.
The very first thing you should do is call your doctor or midwife. They are the experts, and they’ve seen this before. They will advise you to stop taking the birth control immediately and will schedule your first prenatal appointment.
During your appointment, they will discuss your history, confirm the pregnancy, and talk about the next steps for your prenatal care. They’ll be able to reassure you based on the information you provide about the type of birth control you were using and for how long.

What If IUDs are Involved?
As mentioned, IUDs work differently. If you get pregnant with an IUD in place, it's a bit like having a tiny roadblock in your uterus. While many pregnancies with IUDs go on to be perfectly healthy, there is a higher risk of complications, including ectopic pregnancy (where the pregnancy implants outside the uterus, which is a medical emergency) and miscarriage. This is why doctors usually recommend removing an IUD if a pregnancy is detected.
It’s a more delicate situation, and professional medical attention is absolutely crucial. It’s like finding a small pebble in a delicate machine – you want an expert to gently remove it so the machine can function properly.
The Bottom Line: Don't Panic!
The main takeaway from all this is that if you accidentally take birth control when you’re already pregnant, especially hormonal birth control, the odds are very good that both you and your baby will be absolutely fine. The key is to stop the medication and seek professional medical advice as soon as you know.
It’s a testament to how our bodies are incredibly resilient and how the science behind reproductive health is constantly evolving. So, while it might seem like a weird or even scary situation, it’s generally a scenario with a very positive outcome. Stay curious, stay informed, and always chat with your healthcare provider!
